Elephantiasis
Elephantiasis (Facts and History)
Overview
Elephantiasis is a common term for either Lymphatic filariasis or Podoconiosis.
These are two different diseases but they both cause enlargement of lower extremities that would appear like an elephant’s limb and thus accountable for the term. Both diseases are included in the list of Neglected Tropical Diseases by the World Health Organization. [1]
Lymphatic filariasis
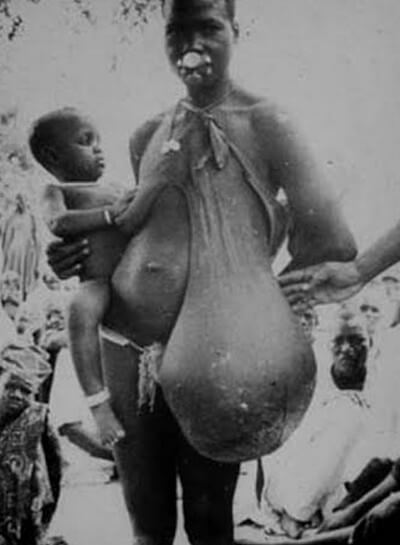
Lymphatic filariasis is an infectious disease caused by nematodes (roundworms) that are spread to humans by mosquitoes. The most noted characteristic of this disease is the profuse enlargement of one or both limbs, one or both breasts in women, areas of the face, and genital area due to fluid accumulation and lodging of the parasites in the human lymphatic system.
Podoconiosis
Elephantiasis also occurs without the role of parasites. The nonparasitic form is termed as Podoconiosis or Endemic Nonfilarial Elephantiasis. It is thought to be caused by constant contact with certain irritant soils specifically red clays that contain very high amounts of alkali metals including potassium and sodium, and other volcanic minerals.
However, not everyone who is in constant contact with the soil acquires the disease. Hence researchers conclude that there is a predisposing genetic factor for the patients’ susceptibility to the disease.
Unlike Lymphatic Filariasis, Podoconiosis only affects the lower extremities since they are the parts in constant contact with the mentioned soils then the swelling continues in an ascending manner. The swellings are always bipedal though they can be asymmetric.
The skin of the affected foot may develop thickenings and bumps (hyperkeratotic papillomata) hence Podoconiosis is also commonly termed as Mossy Foot.
Causes of Elephantiasis
Lymphatic Filariasis
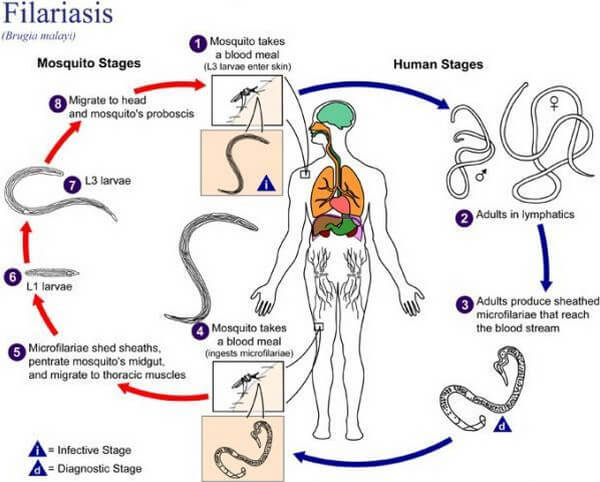
Picture 1 : This diagram shows the cycle of Lymphatic filariasis infection. Parasites are transmitted from one person to another by specific mosquito species which serves as carriers for the parasites.
Source: sciencedaily.com
The causes of Lymphatic filariasis are nematodes of the family Filariodidea. These include Wuchereria bancrofti, Brugia malayi, and B. timori. Of these three species, Wuchereria bancrofti is the cause for 90% or most of filariasis cases.
These parasites are transmitted by different types of mosquitoes that act as vectors. They include:
- Culex mosquito, widespread across urban and semi-urban areas
- Anopheles, mainly in rural areas
- Aedes, mainly in endemic islands in the Pacific.
When an infected mosquito bites a person, the larvae are deposited on the person’s skin wherein they enter the body. The larvae then migrate to the lymphatic vessels where they develop into adult worms.
Mature nematodes live for about six to eight years. Within their lifespan, they lay millions of eggs that hatch into microfilariae or small larvae would also circulate in the bloodstream.
Infection is usually acquired in childhood, but it is in later life that the painful and profoundly disfiguring visible manifestations occur. The disease may cause temporary disability in acute episodes or may lead to permanent disability. [2, 3, 4]
Podoconiosis
Lymphatic Filariasis was thought to be the sole cause of Elephantiasis until the 1970’s when a British surgeon, Ernest W. Price, observed that patients on tropical high altitude areas don’t have evidences of nematodes in their lymph nodes. [6]
Instead, Price discovered micro-particles inside macrophage cells. These microparticles were identified as soil minerals such as aluminium and silicon which displayed adherence to lymphocyte surfaces.
According to Price, the microparticles enter the body via the skin and are “clogged” in the lymphatic vessels. Being foreign bodies, they attract lymphocytes causing subendothelial edema. This is then followed by the lumen’s collagenization which then leads to complete blockage. [5]
Studies show that this disease depends on a predisposing genetic condition that causes the abnormal reaction to these minerals found in red clay soils. [6]
Symptoms of Elephantiasis
Manifestations of Lymphatic filariasis
- Asymptomatic. This occurs in the most cases. The superficial signs are not observed but the parasites would still damage the lymphatic circulation, the kidneys, and the immune system.
- Acute. This includes periods of inflammation locally involving the skin, and the nodes and vessels of the lymphatic system. The inflammation is often accompanied by tissue swelling or chronic lymphedema. The swelling is often related to the body’s immune reaction to the invading parasite. However, normal immune defenses may be impaired due to lymphatic damage; this is manifested by bacterial infection on the skin of affected areas.
- Chronic. When the disease develops as a chronic condition, skin/ or tissue swelling and thickening would involve the entire limb and there would be fluid accumulation or hydrocele in the affected area. The skin of affected areas usually become pebbly and darkened in appearance and may also be ulcerated. The breasts and genital area are also commonly affected.
Manifestations of Podoconiosis
- Early symptoms generally include itching on the forefoot’s skin followed by a burning sensation up to the lower leg. Early changes also include forefoot splaying, plantar edema accompanied by lymph ooze, hyperkeratosis or roughening of the skin, formation papillomata, and rigidity of toes.
- Late symptoms. The disease has a prodromal period prior to elephantiasis. When elephantiasis sets in, the patients may experience two types of swelling: soft or hard. Soft or fluid swelling is followed by hard fibrotic swelling which is accompanied by hard nodules on the skin. Acute adenolymphangitis occur in episodes wherein patients develop fever and their limbs become warm and painful.
Diagnosis of Elephantiasis
The differentiation between the two diseases starts with the patient’s profile.
His/her geographical place of residence gives a pertinent clue. Lymphatic filariasis occur in low lying areas (less than 1500 m or 5000 ft above sea level) while Podoconiosis occurs in high altitude areas (greater than 1500 m or 5000 ft above sea level).
Taking a look at the symptoms, Lymphatic filariasis progresses in a descending manner, usually starting at the groin then down to the limb. The swelling usually affects only one limb. Podoconiosis, on the other hand, progresses in an ascending manner starting from the feet upwards. Swelling affects both limbs but rarely reach above the knee area.
Diagnostic techniques are also available. Non-reactivity of the sample to immunologic tests confirms that the elephantiasis is of non-filarial type.
Pictures and Images of Elephantiasis
Lymphatic Filariasis Pictures

Picture 2: Lymphatic filariasis is often manifested as swelling and thickening of one or both lower limbs (Image on the left). Affected areas are sometimes accompanied with bacterial infections as in the case of the image on the right displaying a patient with both limbs affected
Image Sources: newspakistan.pk ; dermaamin.com
.


Picture 3: The genitals are also commonly affected. The first picture shows an infected vulva that would be surgically removed. The second image shows infected scrotum.
Image Source: documentingreality.com; bjui.org

Picture 4: Other areas may also be affected such as areas of the face and either or both breasts in females. The image below displays a patient with a swollen eyelid and the image on the right shows a woman with affected breasts.
Photo Sources: webeye.ophth.uiowa.edu ; umvf.univ-nantes.fr
Podoconiosis Pictures


Picture 5: The image above shows an early stage of Podoconiosis. Mild splaying occurs and the skin becomes roughened with papillomata. The image below shows the fibrotic stage wherein hard nodules develop on the skin as a result of connective tissue abnormality.
Image Source: actiononpodo.com

Picture 6: The image shows a late stage of Podoconiosis wherein there is bipedal swelling and hyperkeratosis.
Photo Source: actiononpodo.com
Treatment and Prevention
Lymphatic Filariasis
- Mass Drug Administration – The WHO recommends MDA or Mass Drug Administration for the treatment of Lymphatic filariasis. It is a combination of two antihelminthic drugs that are taken in a single dose. This combination eradicates microfilariae from the bloodstream.
There are two formulated combinations consisting of Albendazole which is combined with either Ivermectin or Diethylcarbamazine citrate. - Surgery – In terminal cases of Elephantiasis, surgical procedures are done to cure hydrocoele and reconstruct affected areas.
- Mosquito Control – Since mosquitoes are the vectors for parasites that cause Lymphatic filariasis, mosquito control is a vital step to prevent transmission. Means of control include insecticide-treated nets and indoor residual spraying.
- Hygiene – For infected patients, vigilant hygiene should be maintained to prevent aggravation and secondary infection. Proper exercise is also encouraged for proper circulation thus to prevent lymph accumulation. [2]
Podoconiosis
- Wearing of protective footwear – Unlike Lymphatic Filariasis, the prevention of Podoconiosis is less expensive and is quite simpler. The mere wearing of protective footwear is already efficient to prevent or minimize constant contact with the irritant soil. According to Dr. Price, the disease was also prevalent in some highlands of North America and Europe but was eliminated since the advent of wearing footwear. [5, 7, 8]
- Foot-washing with soap and water – This regimen includes daily washing of the feet with soap and water. Bleach is commonly added to the water to decrease the bacterial burden of the feet and to keep them hydrated. Other antiseptics may also be used.
- Use of antibacterial emollients. – Simple inexpensive antibacterial emollients, such as Whitfield Ointment, provide two benefits for the patient. First, they reduce microbial growth on the infected skin. Second, they also keep the skin hydrated and thus reduce friction and cracking while promoting skin turnover (thickened skin will be replaced by normal new skin cells).
- Reduction of swelling – Bandaging of affected areas to induce compression is effective in minimizing the size of swelling. Elevation of the affected area also does the same. Exercise may also be beneficial since it induces proper circulation.
- Surgical removal of nodules – Usually, only prominent nodules are being removed since the course of the disease is highly reversible. Radical surgery is not recommended. [6, 7, 8]
References:
- http://www.who.int/neglected_diseases/diseases/podoconiosis/en/
- http://www.who.int/mediacentre/factsheets/fs102/en/
- http://www.who.int/lymphatic_filariasis/epidemiology/en/
- http://www.thiswormyworld.org/blog/mapping-of-lymphatic-filariasis-and-podoconiosis-in-ethiopia
- http://www.ncbi.nlm.nih.gov/pubmed/653784?dopt=Abstract&report=docsum
- http://www.podo.org/about-podoconiosis/
- http://mossyfoot.com/index.html#/podoconiosis/
- http://www.actiononpodo.com/about-podoconiosis.html
Also see : Swollen Feet and Ankles – Causes and Treatment
Published by Dr. Raj MD under Diseases and Conditions.
Article was last reviewed on August 6th, 2018.

