Temporal Arteritis
What is Temporal Arteritis?
Temporal arteritis refers to the condition in which there is an inflammation or damage of the temporal arteries in the brain which are responsible for the blood supply of the head and brain [1].
This disorder particularly affects the large and medium arteries which are branching from the neck area [2]. The temporal arteries run to the temple areas which are next to the eye.
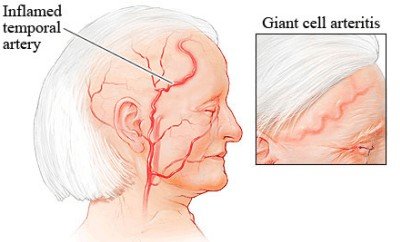
Picture 1: Image of an inflamed temporal artery
Image Source: webmd.com
Some experts identify it as an autoimmune disorder in which the immune system mistakenly identifies the normal health cells and tissues as something that threatens the body. As a result, it attacks the body’s cells and tissues. Thus, it causes inflammation, particularly to the temporal arteries but may also damage the other arteries throughout the body. [3]
Most often, older adults who are aged 50 years and above can develop this condition. Though there may be instances in which it may occur in younger people. Also, women have twice chances of having this condition compared to men. Many cases of temporal arteritis are prevalent in white people, specifically those who are Northern Europeans. However, it can develop across the world and in any ethnicity. Annually, the incidence of this condition reaches approximately 18 cases for every 100,000 people who are above 50 years of age. [4]
Temporal Arteritis Causes
The exact cause in which temporal arteritis occurs is still not entirely understood [5]. Normally, the arteries are described as pliable tubes with walls which are thick and elastic. The blood carrying oxygen leaves the heart through the aorta, the body’s main artery.
Aorta is then divided into smaller arteries which supply blood to all of the body parts, including the brain and other organs.So, when a condition causes the arteries to be inflamed, these arteries will be swollen.This will lead to compromised blood flow throughout the body. In this condition, the large and medium-sized arteries particularly those in the head, the temporal arteries, are mainly affected. The temporal arteries run over the areas from the front of the ears and continue up to the scalp. [6]
Here are some of the associated factors which may cause the occurrence of this condition:
1. Autoimmune response
- The current theory regarding the cause of the temporal arteritis involves the body’s maladaptive response when endothelial injury occurs.
- According to the researchers, the inflammation of temporal arteries results from the inappropriate activation of cell-mediated immunity. When this happens, the cytokines will be released into the arterial vessel wall. This will cause the body’s immune system to become activated.
2. Infectious diseases
- There are some studies which suggest that some infectious pathogens may contribute to the occurrence of temporal arteritis though the role that they may play to the development of the disease is unclear.
- These include microbial pathogens such as Chlamydia species and Parvovirus B19.
- Other infectious diseases associated are hepatitis B, influenza, and Borrellia burgdorferi infection.
3. Genetics
- Some genetic components also contribute to the development of temporal arteritis.
- Alleles, particularly the human leukocyte antigen HLA-DR4 and HLA-DRB104, are believed to increase a person’s susceptibility to the temporal arteritis.
Temporal Arteritis Symptoms
The clinical symptoms of temporal arteritis occur as a result of the affected arteries’ inflammation. These include:
Pain and Tenderness
1. Headache
- This is considered to be the most usual chief complaint of patients with temporal arteritis.
- It is described to be sudden in onset with localization to the temporal region. Though there are also cases in which the headache occurs diffusely that affects the frontal, parietal, or occipital regions.
- Every occurrence of headache has a tendency to be new or different in quality than the previous headaches.
- Also, it can be burning or lancination in terms of sensation.

Picture 2: Area where headache associated to temporal arteritis is felt
Image Source: vision-and-eye-health.com
2. Scalp tenderness
- This is present in about more than one fourth of the temporal arteritis patients. Usually, this accompanies headache but may also appear by itself.
- It is most commonly felt where the temporal or occipital artery is. The affected arteries may be found as nodular, swollen, or erythematous. Also, there may be decreased temporal artery pulse noted.
- There are cases in which there may be an involvement of superficial temporal artery. This results to severe scalp tenderness during simple actions such as combing hair, resting head on the pillow, or wearing eyeglasses or hats.
- Severe cases of scalp tenderness may lead to appearance of scalp necrosis.

Picture 3: Scalp necrosis
Image Source: rheumatology.org
3. Jaw claudication
- Another common finding which is brought by the inflammation of maxillary artery.
- Activities such as chewing and speaking may induce pain felt unilaterally on the affected side or bilaterally.
4. Pain and blanching of the tongue
- This occurs due to the involvement of the lingual artery.
- There are also rare instances in which this may result to tongue gangrene.
Eye problems
The ocular symptoms of temporal arteritis usually affect one eye initially. Later on, the second eye becomes involved in a span of 1 to 10 days.
1. Initial visual problems
- In the early stages, visual problems include diplopia and partial loss of vision. These symptoms are described as transient and intermittent.
- However, if these initial visual symptoms are untreated, it may lead to permanent vision loss.
2. Permanent blindness
- A condition called anterior ischemic optic neuropathy may result due to the inflamed arteries which supply blood to the eyes.
Neurologic symptoms
The symptoms involving the neurologic system are manifested in approximately 30% of people who are with biopsy-proven temporal arteritis.
1. Neuropathies
- This occurs due to the occluded nutrient arteries.
2. Hearing problems
- Problems with hearing are associated to the compromised blood supply to the arteries of the otic region.
- As a result, vertigo, tinnitus, and hearing loss may be experienced by a temporal arteritis patient.
3. Thoracic aortic aneurysyms
- This condition is associated by the presence of systemic vascular diseases, just like temporal arteritis.
4. Other neurologic disorders
- Includes transient ischemic attacks (TIA) as well as strokes brought by vertebrobasilar or carotid disease
Symptoms occurring due to systemic involvement
- Fever
- Fatigue, malaise
- Weight loss due to anorexia
- Depression
- Polymyalgia rheumatic symptoms may also be present
According to the 1990 Americal College of Rheumatology criteria, in order to be diagnosed with temporal arteritis, at least 3 of the following items must be noted in the patient:
- Patient who is 50 years or older at the onset of the disease
- Manifestation of headache which has a new onset or type of localization
- Tenderness of the temporal artery upon palpation and decreased temporal artery pulse which are not associated with arteriosclerosis of the cervical arteries
- Increased ESR than 50 mm per hour using the Westegren method
- Biopsy specimen of the artery which shows vasculitis that is characterized by pre-dominant granulomatous inflammation or mononuclear cell infiltration [4, 5, 7]
Temporal Arteritis Exams and Tests
Laboratory Tests
1. Elevated Sedimentation Rate (ESR)
- This is the most common laboratory test which is used for diagnosing temporal arteritis. Its main purpose is to mark the presence of inflammation. Patients who are with this condition have an ESR of greater than 80 mm/h. However, there are patients diagnosed but have a low or normal ESR.
2. C-reactive protein (CRP)
- This is another diagnostic test which is useful in determining presence of inflammation. It specifically measures the level of C-reactive protein (CRP), a substance produced by the liver when there is inflammation.
3. Liver Function Tests
- This test is indicated to show the mild abnormalities in patients with temporal arteritis. A common finding in this test is elevated alkaline phosphatise level.
4. Complete blood count (CBC)
- Usually, the findings in CBC may reveal low red blood cell count as well as elevated white blood cell and platelets.
Diagnostic Exams
1. Biopsy
- This is considered to be the best way to confirm the diagnosis of temporal arteritis. It is done by obtaining a small sample (biopsy) of temporal artery. For patients with this disease, the results will reveal abnormally large cells.
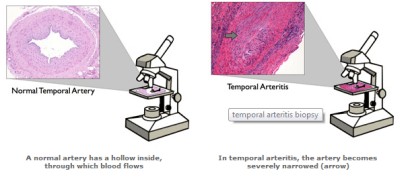
Picture 4: Tissue obtained for examination of temporal arteritis
Source: brighamandwomens.org
2. Magnetic Resonance Imaging (MRI)
- It is a procedure which utilizes a contrast material for the visualization of the blood vessels in the head part.
3. Positron emission tomography (PET)
- A PET scan is very useful in obtaining images of the blood vessels to determine the areas of inflammation. It uses an intravenous tracer solution with a small amount of radioactive material.
4. Doppler ultrasound
- This is done to have visualization of the blood flowing through the veins. [4, 5, 6]
Temporal Arteritis Prognosis
Most of the patients with temporal arteritis are able to recover fully with treatment. However, there are some who needs long-term treatment which may last 1 to 2 years. The need for prolonged treatment is based on factors such as female sex, older age at time of diagnosis, higher baseline ESR, and initial rapid reduction of prednisolone dose. According to patients, relief from symptoms is experienced with treatment. There are also possibilities of spontaneous relapses which may occur within the first years of the disease. [8, 9]
References:
- http://www.healthline.com/health/temporal-arteritis
- http://www.nlm.nih.gov/medlineplus/ency/article/000448.htm
- http://www.localhealth.com/article/temporal-arteritis
- http://www.aafp.org/afp/2000/0815/p789.html
- http://emedicine.medscape.com/article/809492-overview#a0104
- http://www.mayoclinic.com/health/giant-cell-arteritis/DS00440/DSECTION=causes
- http://www.gpnotebook.co.uk/simplepage.cfm?ID=322240516
- http://www.patient.co.uk/doctor/giant-cell-arteritis-temporal-arteritis-pro#
- http://www.nlm.nih.gov/medlineplus/ency/article/000448.htm
Published by Dr. Raj MD under Diseases and Conditions.
Article was last reviewed on August 6th, 2018.

